0 Comments
AUTHOR: NICK + SARAH
INSPIRATION: |
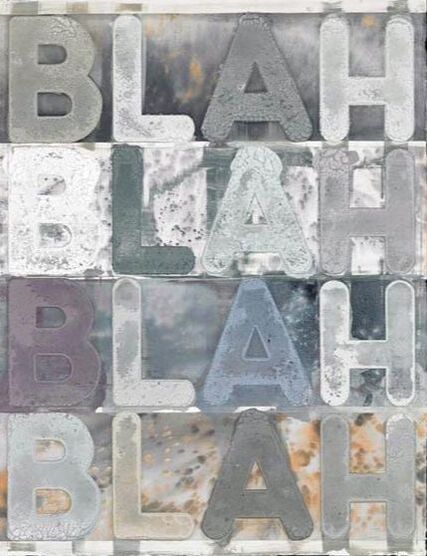
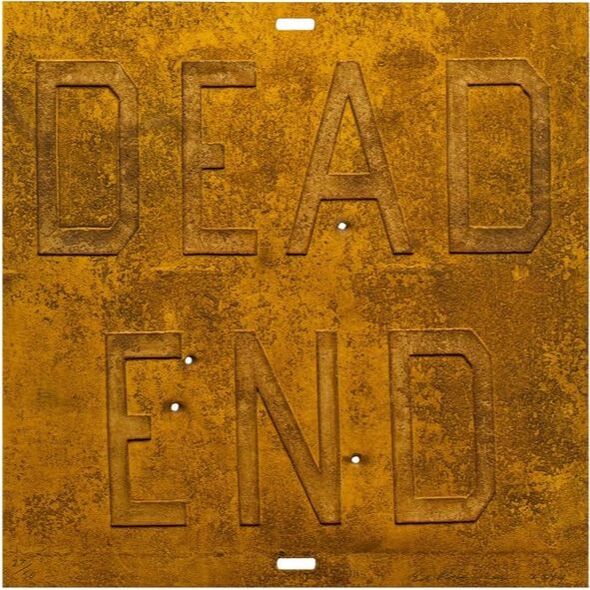
Here are some of my favourite examples: CHRISTOPHER WOOLMEL BOCHNERED RUSCHAJASPER JOHNSAUTHOR: SARAH |
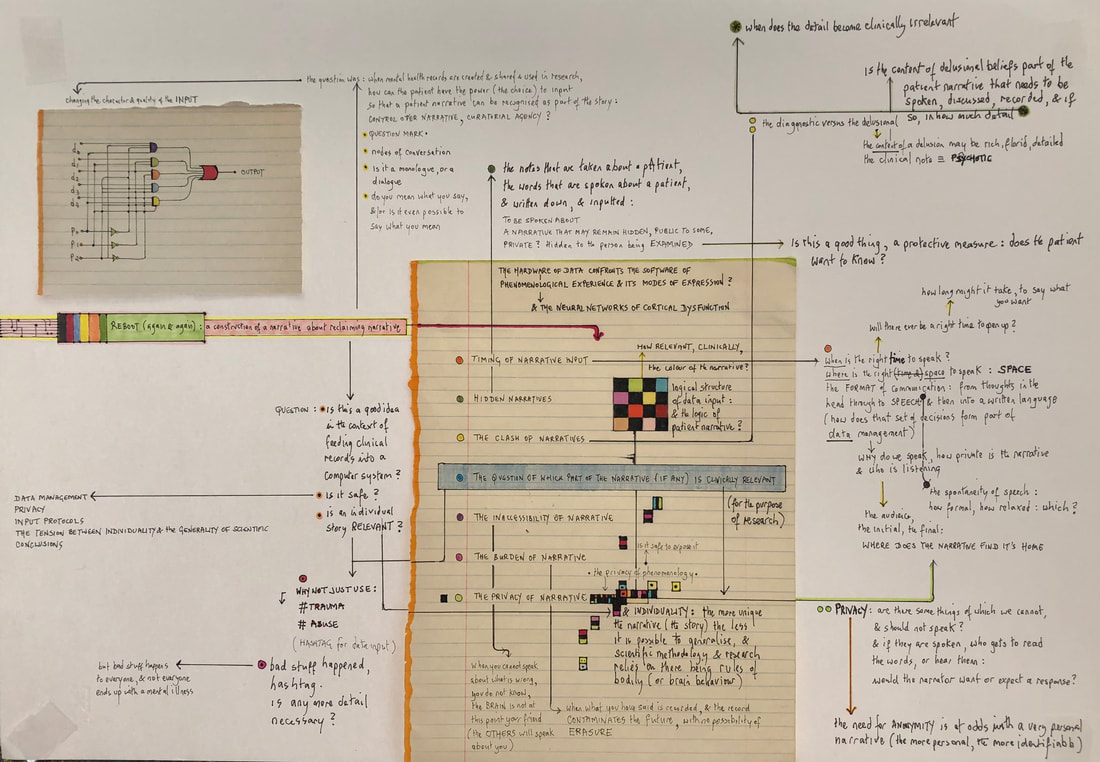
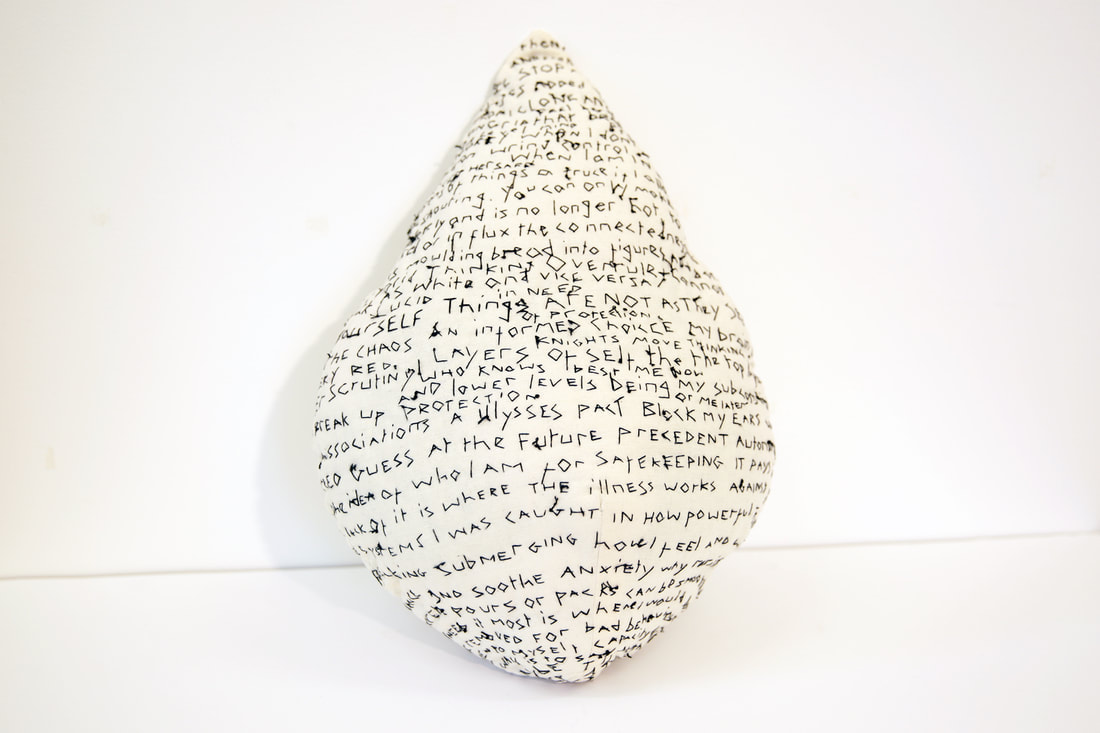
| Beth Hopkins is a fellow artist researcher and friend. We are both currently part of a peer group called the BARP'S (Bethlem Artist Researchers Peer Group) There are many overlaps in our work, so we sometimes record informal chats sharing our findings, ask questions and generally get lost in conversation. Here we talk about this project and how it connects to other work that we are currently involved in: Image Credit: Beth Hopkins. AUTHOR: BETH & SARAH |
"I AM" |
AUTHOR: SARAH
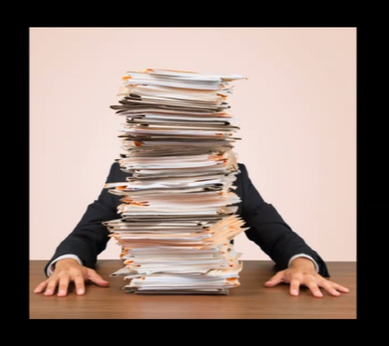
QUOTES: BAKITA KASADHA
| During this R&D period of our project, we have been amassing a treasure trove of ideas and opinions around the experience of the patient narrative. A few weeks ago, we arranged to spend time exploring this area further with the Data Linkage Service User and Carer Advisory Group which was set up to provide Patient and Public Involvement (PPI) for mental health data linkage projects using CRIS data. We had provided the group with some questions in advance mostly to largely suggest some focus for discussion. These were: 1. What does ‘patient narrative’ mean to you? 2. What are your expectations about how and how much of your narrative is captured in the clinical record? 3. If you feel that your narrative is captured sufficiently, what is it that makes it so? 4. Is it important for your narrative to be captured in the clinical record or do you feel that being heard and understood during the consultation is enough? 5. How do you feel about methods to capture the patient narrative such as audio/video recordings? What other means might enhance this process considering, among other issues, ethics, and accuracy? In response to ‘what does ‘patient narrative’ mean to you?’, a group member said that it was their story, their journey of fighting mental illness and fighting the system. Their experience was that of not being listened to particularly around medication and side effects. The shortness of psychiatry consultations meant that the experience is a fire-fighting exercise. Having multiple psychiatrists over your journey can mean that a lot of your personal narrative is lost. We reflected on the fact that this issue of a lack of continuity is important and challenging in a mental healthcare system. What we were hearing was that people had progressed in their journey despite the inconsistent care that has been provided, and that they have developed skills to move forward while not feeling listened to. This is not captured at all or identified in current narratives, of course. As you can track or categorise ‘progress’ in different ways (e.g., hospital criteria) identifying it becomes even more complex. We discussed how CRIS can inform better patient care through its use as a research database. But when we talk to service users, a lot of them are dissatisfied with the patient care throughout their journey. Maybe they have a good clinician at some point, but the negative experiences of the journey are still there. If we could collect people’s narratives and distil information out of that, it would ensure more consistency. The group expressed its appreciation for the work we are doing on highlighting the patient narratives, which may help to give voice to a part of the service user experience that is largely in the shadows. A group member said there were lots of positive things going on in the South London and Maudsley NHS Trust where patients can express themselves through different media, but this is not always captured or put into the record. If it was captured, it could improve the patient’s wellbeing and also have benefits for other patients. If things were documented differently, what would that look like? The group discussed how there had to be a fine line between capturing enough information to be heard, but not too much which might risk details being overlooked. The amount of time you have available to talk was deemed important – as a patient, we pick out the key points of the story and the clinician records that, rather than considering the whole story. The group reflected that the whole story should be listened to, rather than just the highlights. What is more important: to have a lot of data of our narrative which encapsulates the whole story but may have errors, or to have a shorter snapshot which may be more accurate? A group member said the latter was best, as nothing is worse than misinformation recorded in the record which can then follow you throughout life. If one statement is put on someone’s record, others take it at face value. Having it redacted is technically possible but could be a very difficult and lengthy process. Often the statement will be edited rather than removed. This said a lot about power and control of the narrative. These errors might not be malicious and come from a misunderstanding, but they follow us and means it is our word against theirs. Unless we our record or happen to find out, we might not know what misunderstandings/gaps are in our narrative. A comments section in the record could help with this. Insightful, warm and eye-opening. We visited the group with the intention of unpicking the layers that make a good patient narrative; the small and large details that could contribute to a better representation of what it is that we go through as service users. Suffice to say that our questions felt unimportant and secondary as a poignant issue was brought to light. How can you capture or facilitate a better patient narrative when so many people feel that their fragmented experience has stripped them of the chance to have any narrative at all? AUTHOR: ANNA |
MY BACKGROUND IN DANCEI started dancing at the age of three and have always found movement to be an intuitive, instinctual and natural way to communicate. I was a dance teacher and choreograpaher at the start of my career before I began to work as a visual artist and this certainly feeds into my work in many ways. At college, I studied dance and part of the training was in Labanotaiton (a system of recording human movement using a series of symbols). How does this relate to our project? Im thinking of nonverbal communication and how movement might be documented as a valuable form of communication. I wanted to revisit Labanotaion as a form of language and when I did, I found this great YouTube course which explains the basics: What form of communication makes you feel best understood? AUTHOR: SARAH |
| I ask the question "As a patient, do you feel that your narrative is being captured sufficiently within a clinical setting?" One persons experience of having her narrative lost in translation : What is your experience? AUTHOR: SARAH |
BETHLEM ARTISTS RESEARCH PEER GROUP
| Today Anna was welcomed into our weekly drop in. Some of the interesting themes that arose from the discussion were: - Phobia of data (the narrative surrounding this) - The title: Electronic Patient Journey system (great name indeed!) - The parallels with deconstructing and reconstruction in my art practice and with the data (a process of learning for both the machine and I?) - Asking questions in multiple ways in order to be more inclusive. - The idea of the value model - looking at pros vs cons of documenting narrative in different ways - Being given the option in the moment to document your own story. - Editorial / shorthand/ note taking - Offering confirmation that you have understood what someone tells you (a classic teaching technique and also used in metacognition testing) “so what I hear is..... is that correct?” Image: Sarah Carpenter darkroom experimentation AUTHOR: SARAH |
SPEAKING, LISTENING AND HEARINGHow can you possibly look at storytelling without thinking about listening? One message that stands out to me in this podcast is that we can often be solution driven rather than actually listening. Is this what is happening in clinical settings? Is that why our narrative is being lost? Imagine clinicians having the time to listen rather than record! AI could play a part in that. AUTHOR: SARAH CARPENTER |
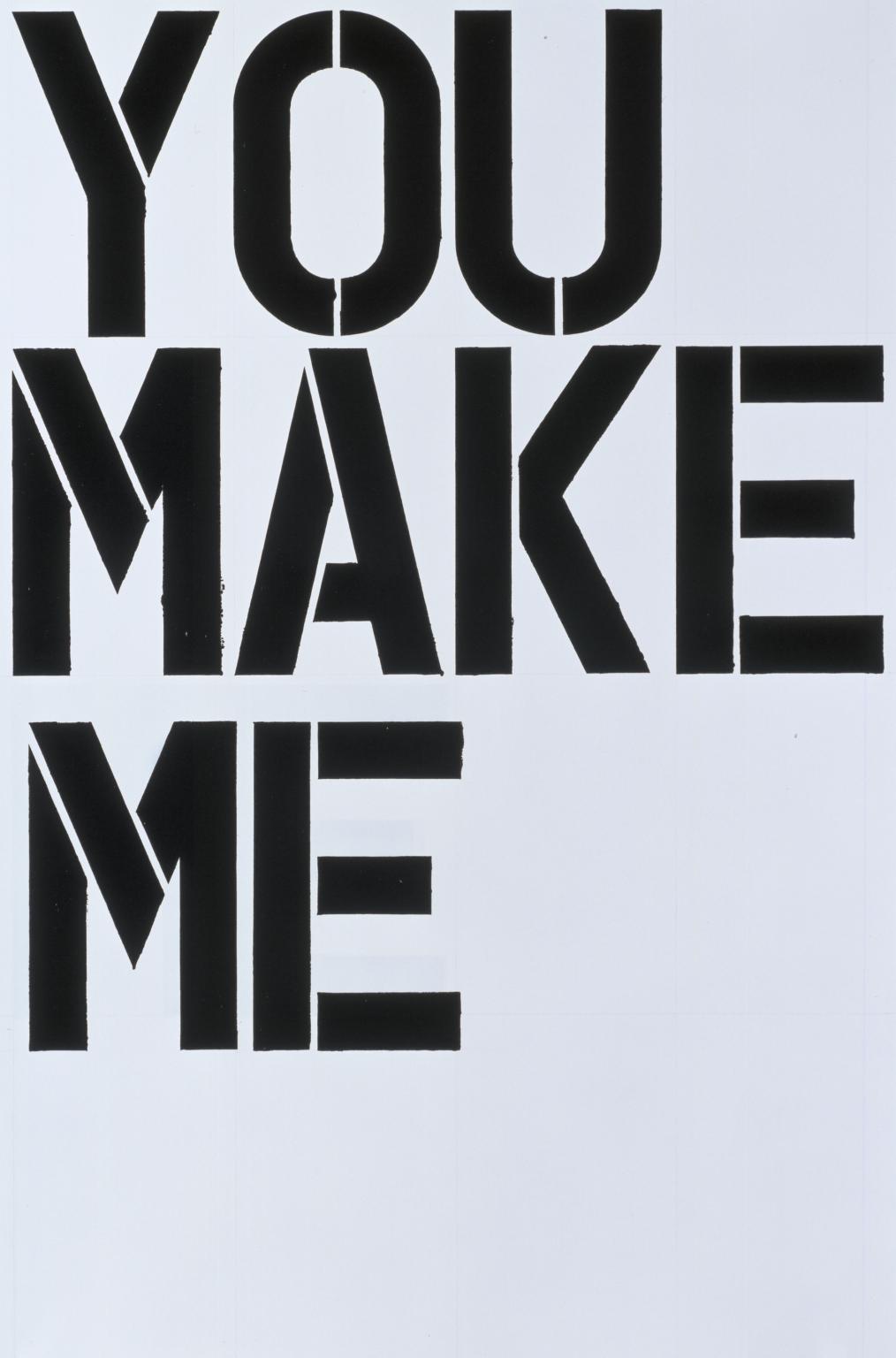
| As part of an interview process, I was asked to chose an object that represented power to me. I chose a blank sheet of paper. I was given 2min to discuss my choice: Having space to write your own narrative = having power. |
AUTHOR: SARAH
CREATIVE RESEARCH
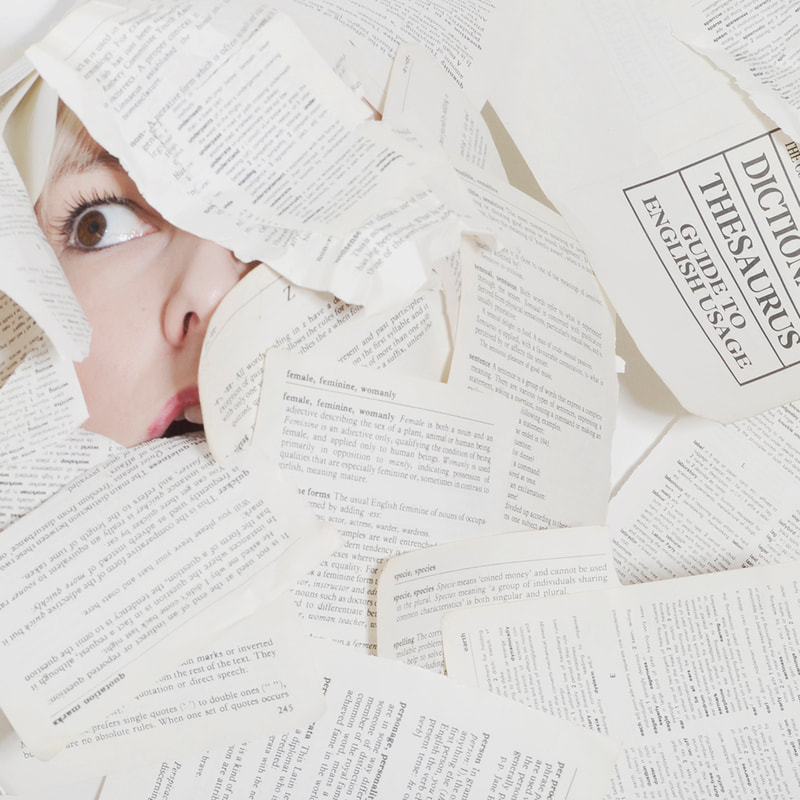
PAPER MAKING
| Deconstructing and reconstructing my records. Creating a fresh blank page ready to tell my own story in my own way. The story so far... |
AUTHOR: SARAH
MEDTECH ENTREPENEURSHIP PANELPANELISTS: The most interesting part of this discussion in relation to this project, was listening to Dr Emilia Molimpakis talk about neuroscience, linguistics and her video gaming system called Thymia. Probably best to just show the 3min video of her explaining it much better than I could in a full blog post (the power of creative/ video storytelling!) ... AUTHOR: SARAH |
BUILDING HEALTHCARE AI FOR THE REAL WORLDSPEAKER: TOM DYER, BEHOLD.AIA really interesting talk thinking about AI vs. Humans and computers replicating and replacing human processes.
In research, the outcome is often measured as human performance vs. AI, so essentially can it be proven that AI is as good or better than humans? Dyer demonstrated that the combination of AI plus human performance always gives better results than either AI or humans can produce alone. The question is how can we work with AI to improve existing processes and complement human skills? Dyer spoke of the narrative of AI in the media: The reoccurring theme of robots being a threat to human beings, they will take our jobs and eventually threaten our very existence by replacing us. Robots are seen as a threat to human beings - we are portrayed as being weaker. Dyer framed things differently, he spoke of AI cooperating with humans, complimenting our skills, being used as a second opinion / cross reference. In terms of diagnosis, AI is easily trained to determine severity of symptoms, and easily and accurately decide if a patient needs either immediate treatment, or no treatment at all. This means that the workload of a clinician can be significantly decreased and more time can be spent on more complex cases that need further analysis. The crucial part of the AI puzzle which is yet to be deciphered, is if the machine sees something unfamiliar. Instead of it saying "I'm not sure", it might automatically place something in its nearest category. These are the instances where we see how vital the clinicians role is and how irreplaceable they are. Imagine though, in a clinical setting, AI taking on the tasks that involve memorising and recalling information (basically what we would define as the 'knowledge" involved), this would mean that clinicians would have more time to engage other important skills such as compassion, empathy and understanding to make a fuller, more rounded diagnosis. This resonated with me and my thoughts on our project. Could this lead to more of the patient narrative being heard and given value in the clinical setting? By allowing better resources for a clinician to utalise their human skills (e.g. compassion), richer and more valuable information might be drawn form from the patient, helping the clinician to make a better assessment. At the same time AI could capture the patient narrative and analyse it using its knowledge. Together, this would provide a more rounded picture of the patient. My mental wellbeing is severely effected by feeling misunderstood. Simply feeling heard is in itself medicine for me. AUTHOR: SARAH |
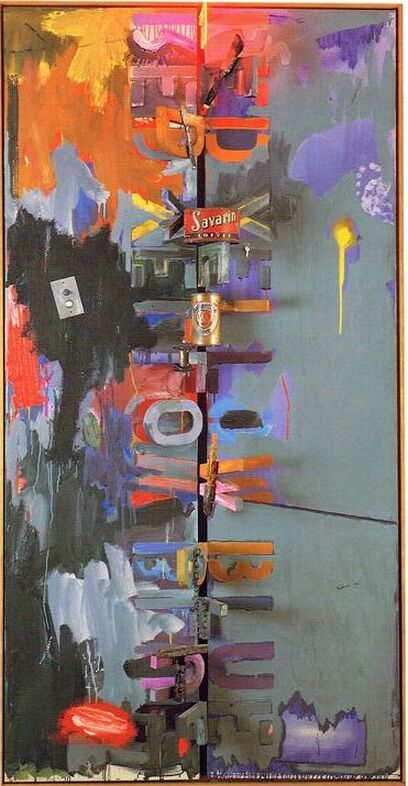
| Acrylic, Collage and Charcoal on cardboard
|
AUTHOR: SARAH
MEDTECH: AI IN MEDICINE SERIES
SPEAKER: DR PEARSE KEANEPearse was absolutely fantastic!
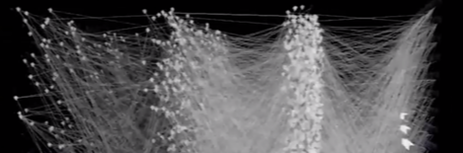
I actually took away a lot of information / ideas from this talk. I think this was because the language used was accessible, communicated slowly and ideas were unpacked for us as if it was the first time we were hearing them (which for me it was!). Thought 1: Until this talk, I hadn't made a direct correlation between the brain and computers. Artificial neural networks as computational methods to replace the brain so in essence, neurons = nodes. Thought 2:
I was fascinated by the work that Pearse is doing that relies on image recognition; computers are fed lots and lots of images, training them to recognise certain things. I recently came across the app Google Quick Draw, it prompts you to draw certain objects and then guesses what you've drawn. It stores the information from each new drawing, uses it to learn and gets better at recognising - the more people interact, the better it becomes. In fact, rather than explain, why not just let you see for yourselves : Thought 3:
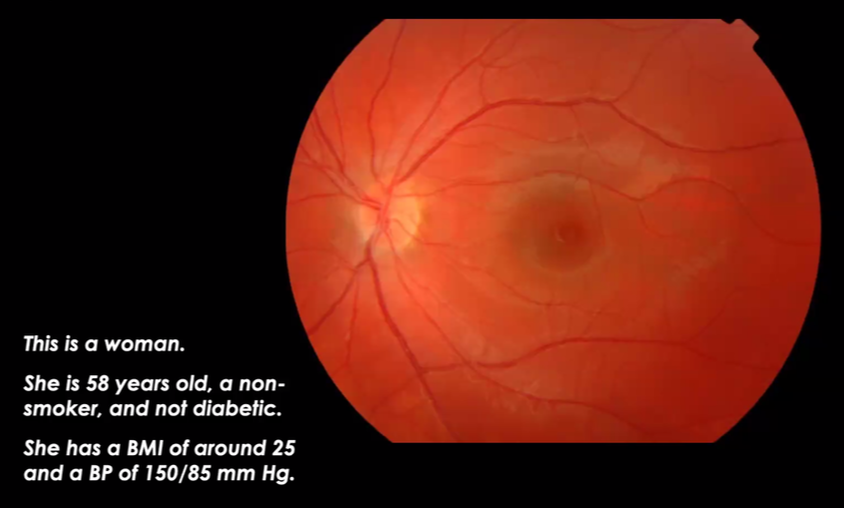
Dr Keane has been doing using OCT scans for the retina (Ultrasounds scans but using lightwaves) to find out all kinds of information about the person such as age and gender etc. I wonder if there's anything the eyes can tell you about a person's mental state? Could MRI scans give us this kind of information about a person? Thought 4:
During the talk I was introduced to the term "AI chasm". This is the difficult gap between imagining a prototype and then actually putting it into action in a clinical setting once it has approval. We're talking years (on average around 8!) How can this be navigated? By the time useful technology is developed and in clinical settings, it's already outdated. Thought 5:
When it comes to coding, Pearse had an opposing view to the last talk, believing that experience in this area is not necessary. I've always felt I should learn to code in order to understand the process, however, I learned today that there are new "drag-and-drop" systems for anyone who wants to have a go at this kind of . This opens up a whole new world of possibilities and makes me feel that I might actually be able to put some of my creative research into action. I must delve deeper into this! TBC... IMAGE CREDIT:
SCREENSHOTS FROM DR PEARSE KEANE'S PRESENTATION AUTHOR: SARAH |
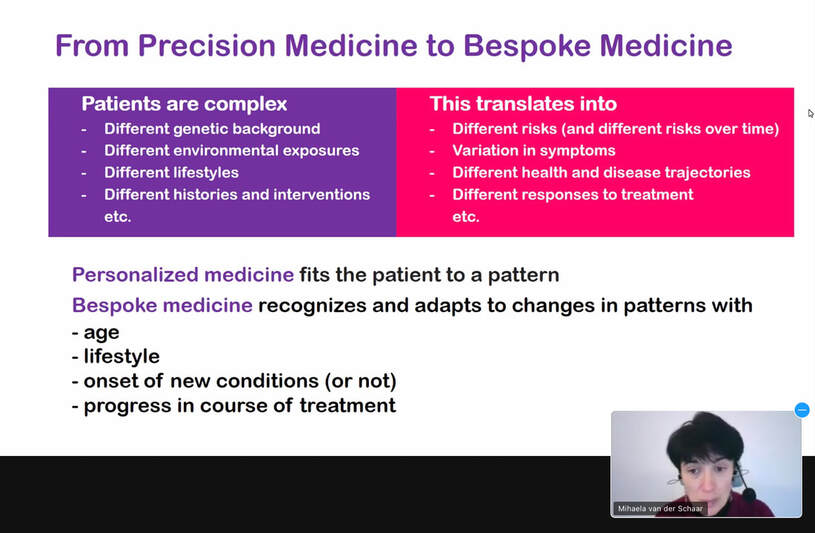
MEDTECH: AI IN MEDICINE SERIES
|
MEDTECH: AI IN MEDICINE SERIES
|
AUTHOR: SARAH
MEDTECH: AI IN MEDICINE SERIES WITH UNIVERSITY COLLEGE LONDON (UCL)So, I’ve decided to engage with UCL's MedTech AI in Medicine series over the next two weeks.
Although I have little / no basic understanding of some of the subject matter, I'm interested to see if I can pick out any information, thoughts, theories from these talks for use in our project. Perhaps I may also meet some speakers who are interested in our project? If nothing else, I am interested in the language that is used to deliver information and how accessible it is for those like myself who have an interest but don't come from a clinical or tech background. I wonder how the use of academic and clinical language might be a barrier when it comes to patients with mental illness sharing information / telling their own story? AUTHOR: SARAH |
AUTHOR
Here you will find blog posts by both Anna and Sarah
ARCHIVES
June 2021
May 2021
April 2021
March 2021
February 2021
January 2021
December 2020
CATEGORIES
All
ACCESSIBILITY
ADVANCED DIRECTIVE
AGENCY
AI
ANNA
ARTWORK
AUDIO
BETH
BETHLEM GALLERY
COLLABORATION
COMPASSION
DECONSTRUCT
DYSLEXIA
EHR
GRAPHIC DESIGN
HEARING
HISTORY
IMAGES
KCL
LABANOTATION
LANGUAGE
LANGUAGE AS SYMBOLS
LISTENING
MEDTECH
NARRATIVE
NICK
PERFORMANCE
PODCAST
POETRY
POWER
PRINTMAKING
RECONSTRUCT
RECORDS
SARAH
SPEAKING
STORY
SUE
VISUAL COMMUNICATION
















 RSS Feed
RSS Feed
